
Karin Gaensler, MD, Professor, Department of Medicine (Hematology/Oncology), and the Krishnamurthi Endowed Chair in Hematological Malignancies at UCSF. Photo by Steve Babuljak
An experimental cancer vaccine in early-stage development at the University of California San Francisco has sparked hope that patients with acute myeloid leukemia (AML), an aggressive cancer of the blood, could one day have a life-saving alternative, especially those prone to relapse or unable to tolerate existing intensive treatments.
“Immune-based therapy is an area of oncology whose time has come.
Scientists and clinicians are building a greater understanding of how immune therapies can bring new possibilities to patients with aggressive cancer for whom prior chemotherapy approaches were not adequately effective.”
-Karin Gaensler, MD
Scientists and clinicians are building a greater understanding of how immune therapies can bring new possibilities to patients with aggressive cancer for whom prior chemotherapy approaches were not adequately effective.”
-Karin Gaensler, MD
By engineering cancer cells into a personalized vaccine tested on models of AML, the team from UCSF’s Helen Diller Family Comprehensive Cancer Center triggered a leukemia-specific immune response that overcame disease- and age-related factors that would otherwise allow residual AML cells to persist after chemotherapy. It is the residual cells that cause relapse and poor outcomes. The team’s novel approach resulted in long-term survival and eradication of AML in mouse models, according to an article published last November in the journal Blood Advances.
The promise of the research and the patient need it addresses were recognized by the California Institute of Regenerative Medicine (CIRM), which awarded Karin Gaensler, MD, and her team a $4.17 million translational grant last October. The funding will allow the team to advance its proof- of- concept studies to the stage where it could initiate early discussions with the U.S. Food and Drug Administration about clinical trials.
“CIRM’s Grants Working Group appreciated the novelty of Dr. Gaensler’s approach targeting cancer stem cells and the design of her CIRM-supported study – including testing her candidate on human patient AML samples - should allow her to translate her work forward towards the clinic,” said Ross Okamura, PhD, CIRM senior science officer.
“Cancer vaccines have been in use for some time, both as a preventative measure (HPV, Hepatitis B), as well as a therapeutic where the vaccine is composed of antigens that can educate the immune system to ward off disease,” Okamura said. “Identifying an antigen to specifically target AML curatively has been difficult.”
There is an unmet need for novel approaches to fighting AML, especially for people over 60-years-old who have higher-risk forms of the disease and/or treatment restrictions that make them ineligible for more intensive therapies, she said. “That’s two-thirds of the 21,500 Americans diagnosed with the disease annually who have an abysmal prognosis, which may be less than a year,” he said.
Age Matters
AML is a rapidly progressing cancer in which the bone marrow makes abnormal myeloblasts, a type of white blood cell that is a precursor to other types of blood cells. As the abnormal cells proliferate, there’s less room for healthy cells, which can lead to anemia, infection and easy bleeding. People young and old are diagnosed with AML, though the average age is 68. Young people with AML fare better than older patients. The five-year survival rate of AML is 27 percent.
About two-thirds of people diagnosed with AML will undergo chemotherapy. Approximately 67 percent of all those patients go into remission, although that number falls to 50 percent for people over 60, according to the National Cancer Institute. Patients who relapse may receive more intensive chemotherapy, radiation, or a targeted therapy that focuses on the genetic mutations driving the disease.
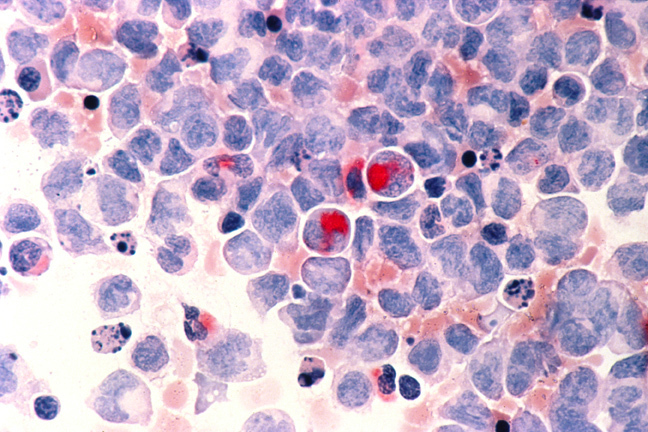
Human cells with acute myelocytic leukemia (AML) in the pericardial fluid, shown with an esterase stain at 400x.Courtesty of the National Cancer Institute
Advancing immunotherapy
Another option that has been used with great success for the past 40 years is a stem cell transplant from a healthy, related or unrelated donor. The transplanted cells reboot a patient’s immune system, making it more effective at fighting off the cancer. “Along with donor stem cells, transplant recipients benefit from the ability of donor’s mature immune cells to recognize and kill residual leukemia cells that are the source of relapse,” Gaensler said. This empowering of the immune system is known as the graft-versus-leukemia effect.
“In acute leukemias, such as AML, the provision of these mature healthy immune cells can increase relapse-free survival and even cure some patients,” said Gaensler, the cancer center’s Krishnamurthi Endowed Chair in Hematological Malignancies. The endowment is funded through a gift to UCSF from the Krishnamurthi family, to honor a family member whose AML was treated there.
The major focus of Gaensler’s lab is the development of a universally applicable vaccine strategy with the potential to improve treatment outcomes, without the risks and toxicities of transplant. The vaccine would be given to AML patients after chemotherapy, with the aim of stimulating the body’s immune response to attack leukemia cells the body may still harbor.
Immune-based approaches to cancer therapy, generally known as immunotherapy, have yielded exciting results in oncology during the past decade. Unfortunately, prior promising AML vaccines have not been reliably successful in extending relapse-free survival.
“A major goal for the development of our vaccine is to stimulate graft versus leukemia-like effects in transplant-ineligible patients,” said Gaensler. “A vaccine that stimulates effective leukemia-specific immunity would also be a breakthrough for patients able to undergo transplantation, as these patients still have a high relapse risk of about 30 to 50 percent.”
The challenge of developing a therapeutic vaccine is making it work for everyone, since everyone’s cancer is unique.
“Much like how a single snowflake can share a similar composition and behavior with another, the exact features of each patient’s leukemia can be different enough to make traditional vaccine approaches useful for only a subset of patients,” explained Okamura, of CIRM.
The UCSF team overcomes this issue by using the patient’s own cancer cells to create a personalized vaccine.
Delivering a one-two punch
AML has characteristics that suppress the immune system, particularly those subtypes typically found in older patients, Gaensler said. Additionally, older patients may have a decline in the responsiveness of their T-cells, which are the workhorses of the immune system.
The UCSF team uses a two-pronged strategy to boost the immune system.
The extracted patient AML cells are modified to express the protein CD80, absent on AML cells, which is required to activate leukemia-killing responses. Without it, T-cells may be unresponsive, allowing the cancer to spread unchecked.
The second part of the strategy is to modify the patient’s leukemia cells to produce an immune stimulatory protein, interleukin-15 (IL-15) in combination with its receptor. IL-15 is uniquely suited to stimulating anti-tumor responses because, when it binds to its own receptor, it stimulates T-cells specifically to become leukemia-specific killer cells, the team wrote in Blood Advances.
Additionally, IL-15 stimulates activation of memory T-cells, potentially increasing the duration of the body’s immune response. IL-15 also stimulates cells in the innate immune system, resulting in natural-killer T-cell activation and proliferation. Gaensler noted that a lot of the research on IL-15 was conducted by George Pavlakis, MD, PhD, from the National Cancer Institute and by Averil Ma, MD, from UCSF.
“The UCSF team’s approach is not susceptible to the cancer mutating a single target antigen since it has educated the immune system to defend against multiple targets; this avoids a common downfall of other immunotherapies,” Okamura said. “More importantly, this approach is designed to attack the cancer stem cells, which if left untargeted, could lead to the cancer returning.”
Next Steps
 The UCSF team is now doing the painstaking work to develop the manufacturing process for the lentiviral vector, which is the method used to engineer the cancer cells. This work includes the strategy for collecting and freezing patient cancer cells. The work, funded by the CIRM grant, is being co-led by Donald B. Kohn, MD, medical director of the Human Gene and Cell Therapy Facility at the University of California Los Angeles. Dr. Kohn will be generating vaccine in protocols that could be used to produce it for human clinical trials, Gaensler said.
The UCSF team is now doing the painstaking work to develop the manufacturing process for the lentiviral vector, which is the method used to engineer the cancer cells. This work includes the strategy for collecting and freezing patient cancer cells. The work, funded by the CIRM grant, is being co-led by Donald B. Kohn, MD, medical director of the Human Gene and Cell Therapy Facility at the University of California Los Angeles. Dr. Kohn will be generating vaccine in protocols that could be used to produce it for human clinical trials, Gaensler said.
Another of the team’s collaborators, Farzin Farzaneh, PhD, of Kings College London, has developed a different AML vaccine and obtained clinical trial approvals in Europe. His work confirms the viability of scaling the process of administering a clinical product without safety of toxicity issues, Gaensler said. “The collaboration of a diverse group of investigators represents and exciting opportunity to pursue novel studies in immune therapy,” she said.
Other members the project consortium include Lloyd Damon, MD, Michael Rosenblum, MD, Lewis Lanier, PhD, Karthik Ganapathi, MD, PhD, Byron Hann, MD, PhD, Ashok Nambier, MD, and William Karlon, MD, all of UCSF, as well as Ravindra Majeti, MD, PhD, from Stanford and William Murphy, PhD, from UC Davis.
If ultimately approved for clinical trials, Gaensler envisions an older patient’s AML cells would be collected at diagnosis. If the initial chemotherapy is successful and the patient goes into remission, he or she would be vaccinated with their own engineered cells. Clinical studies would initially assess safety and then determine whether vaccination stimulates effective anti-leukemic immunity.
“Given that the prognosis for older patients is so poor, and has been for decades, we might know in short time not only about safety and toxicity, but whether there are hints regarding efficacy and immune response,” Gaensler said.
“What we need now is to recruit scientists to help with our studies funded by CIRM and the Leukemia Lymphoma Society, as well as obtaining the necessary future funding to bring novel therapies to clinical trial.”