
Wearing red ribbons in honor of their mentor Dr. Arti Hurria, Drs. Li-Wen Huang and Melisa Wong of the UCSF Older Adult Cancer Care Program discuss the emerging field of geriatric oncology research.
Mentorship within a close-knit community is driving interest in the field of geriatric oncology. Dr. Li-Wen Huang, Hematology Oncology Fellow, and Dr. Melisa Wong, Assistant Professor, Division of Hematology/Oncology, and leader of the new UCSF Older Adult Cancer Care Program, credit key individuals with influencing their career choice to study and treat older adults with cancer.
The late Dr. Arti Hurria, who served as the George Tsai Family Chair in Geriatric Oncology at City of Hope National Medical Center, was one such mentor. After Dr. Hurria’s death in 2018, her peers established and funded in her memory the 2019 Conquer Cancer Foundation of the American Society of Clinical Oncology (ASCO) Endowed Young Investigator Award (YIA) in Geriatric Oncology in honor of Dr. Arti Hurria. Dr. Huang was named the inaugural recipient of the award last month at the 2019 ASCO conference.
Drs. Wong and Huang sat down to discuss the meaning of the award, the growing geriatric oncology community, and the mission to address the unique needs of older adults with cancer.
On Finding Geriatric Oncology
Dr. Wong: Dr. Huang, congratulations on receiving the Conquer Cancer Foundation of ASCO Endowed Young Investigator Award in Geriatric Oncology in honor of Dr. Arti Hurria. What initially drew you to geriatric oncology?
Dr. Huang: When I was in medical school, I gravitated toward the older patients, and I liked how the geriatricians had a comprehensive holistic approach to the patient. They considered how the illness impacted every aspect of the patients’ lives, their social support network, and quality of life.
During my residency at Duke, I also became interested in oncology. My mentor then, Dr. Arati Rao, introduced me to the geriatric oncology community through the biweekly Cancer and Aging Research Group (CARG) phone conferences that Dr. Hurria organized. For me, finding this close-knit, collaborative community with a similar interest was instrumental to encouraging me to pursue this still small but growing field. Dr. Hurria made everyone feel welcomed, and built a community where people helped each other out instead of competing with one another.
Dr. Wong: Dr. Hurria always said the only requirement for joining was a passion or desire for helping older adults with cancer. These phone conferences are also a great forum to get feedback. When I applied for my Conquer Cancer Foundation YIA during my oncology fellowship, I actually presented my proposal on a CARG call and got great feedback from the community. So before you even submit the grant, it's been vetted by the geriatric oncology research community and has been improved based on their feedback.
Dr. Huang's YIA award proposal
Dr. Wong: Can you tell me more about your YIA proposal and what you’re hoping to accomplish?
Dr. Huang: My project is titled, "Understanding the relationship between frailty and cognitive decline after allogeneic stem cell transplantation in older adults.” My mentors are Drs. Michael Steinman and Rebecca Olin. Working with a database of patients that Dr. Olin had collected of adults over age 50 who underwent allogeneic stem cell transplantation at UCSF, the goal of this project is to identify predictors of cognitive decline after transplantation using the CARG geriatric assessment developed by Dr. Hurria.
Cognitive function after transplant is important both for quality of life and post-transplant care. Follow-up care for transplant is so complex with many new medications that it really requires an ability to follow instructions closely. The patients get frequent adjustments to the doses and schedule of their medications, including prophylactic antibiotics and immuno-supressive medications. It’s very important they remember how to take their medications because it directly impacts their health after, and the success of, the transplant.
Currently it is not very well understood which patients are at highest risk. My goal is to see if any of the measures in the geriatric assessment, or overall frailty, can predict who is at hightest risk for cognitive decline.
Dr. Wong: How do you see the results of your research helping patients you see in clinic in every day practice?
Dr. Huang: If we are able to identify risk factors for patients at the highest risk for cognitive decline, it will help with having the risk/benefit discussion with patients so they know better what to expect. It will also help with developing post-transplant care plans. For patients at higher risk for cognitive decline, that care plan needs to be even more rigorous to anticipate what resources they have, and who will help them with managing their medications and all their appointments if they do develop cognitive decline.
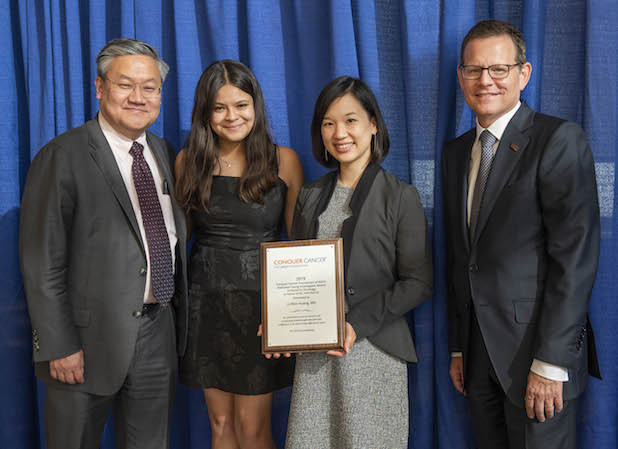
Arti Hurria Endowed YIA recipient Dr. Li-Wen Huang with Dr. Thomas Lee, Serena Lee and Dr. Clifford A. Hudis. Photo by © ASCO/Nick Agro 2019
Dr. Wong: So what does it mean to you to receive not just a YIA award, but this very special one in honor of Dr. Hurria?
Dr. Huang: I can't describe how big of an honor it is to receive the first Conquer Cancer Foundation endowed award in honor of Dr. Hurria. She is someone I've looked up to since the beginning of my interest in geriatric oncology. I know how important she was and still is to the field, and I want to make her proud.
Dr. Wong: One thing we learned from Dr. Hurria is that we really can do a lot more together and get a lot farther together, so you have a whole geriatric oncology community to help you succeed.
Dr. Wong: I received a Conquer Cancer Foundation/Vicky Merryman Women who Conquer Cancer YIA in 2017, and my project looked at chemotherapy-induced peripheral neuropathy in older cancer survivors.
I was interested in seeing how older and younger cancer survivors experience chemotherapy-induced peripheral neuropathy potentially similarly and differently. We found that, on average, older cancer survivors were more likely to have worse objective measures of neuropathy but actually report less interference with their daily activities and lower pain scores. That research really highlighted the importance of both asking patients how they are experiencing different symptoms, and objectively measuring them because there may be differences in how patients experience them. It is important to understand both aspects of it.
I received that award at a very similar time in my early career as Dr. Huang, where I was just about to finish my medical oncology fellowship and my aging-research T32 fellowship in the Division of Geriatrics. It was the first award that I received while I was transitioning to a faculty position. It was a huge honor to have my work recognized outside of my home institution, and that recognition gave me a sense that my work was important. It also showed me that other people see the value in it and are willing to invest in me during this very steep learning curve of gaining more research skills and becoming an independent scientist.
Developing the UCSF Older Adult Cancer Care Program
Dr. Wong: We have developed the UCSF Older Adult Cancer Care Program to try to bring together people from medical oncology, surgical oncology, radiation oncology, physical therapy, nursing, geriatrics, and palliative care especially, to build an infrastructure to improve cancer care for older adults and support our cancer and aging research. A lot of UCSF Cancer Center research is centered around clinical trials in disease groups, but geriatric oncology really crosses all types of cancer. What we can do together is more than what we could have done individually in our silos.
One of our first steps was hosting a Geriatric Oncology Symposium in September 2018, where we invited Dr. Hurria to be our keynote speaker. She gave a great keynote highlighting why geriatric oncology is such an important aspect of cancer research. As the aging population grows, there are more and more older cancer patients, and that means a lot of older cancer survivors as well, and they may have unique needs that a younger population wouldn't. So, we really have to focus on the specific needs of older patients, how their comorbidities, cognition, and other aspects of their lives influence how their cancer is managed, and also how cancer treatment impacts their lives and their ability to take care of themselves.
There are a lot of long term effects of cancer and cancer treatment that can be magnified in older patients. For example, if an older patient has some lingering neuropathy from their taxane chemotherapy, that may increase their risk of falls, which then may result in hospitalization and more functional decline. The consequences of cancer treatments can impact an older person's ability to take care of themselves independently.
There is a growing recognition that many of our UCSF patients are older, and it is our responsibility to take the best care of them that we can. That involves a multi-disciplinary team of geriatricians, palliative care, nurse practitioners, nutritionists, occupational therapists, social workers. We are starting to feel a groundswell of support for putting together a more comprehensive program.
Dr. Huang: In general oncology, we're continually coming up with new exciting therapies, yet older adults, especially those with comorbidities, are often not included in clinical trials. Thus older adults often do not benefit or benefit more slowly from new therapies because we don't know whether or how we can use these new treatments safely in them.
Yet we know our aging population is growing rapidly, so a large portion of our population do not benefit from these advancements. Just because a patient is older doesn’t mean you can't treat them. It may be more challenging treating older patients who have more co-morbidities and also a life-threatening cancer, but that is exactly why we need more people to do research in this field.
Get involved:
The UCSF OACC Program meets bimonthly (even months) on the Parnassus campus and by video conferencing to bring together experts in cancer and aging across all cancer specialties and supportive care programs. To join at the next meeting please email [email protected].
