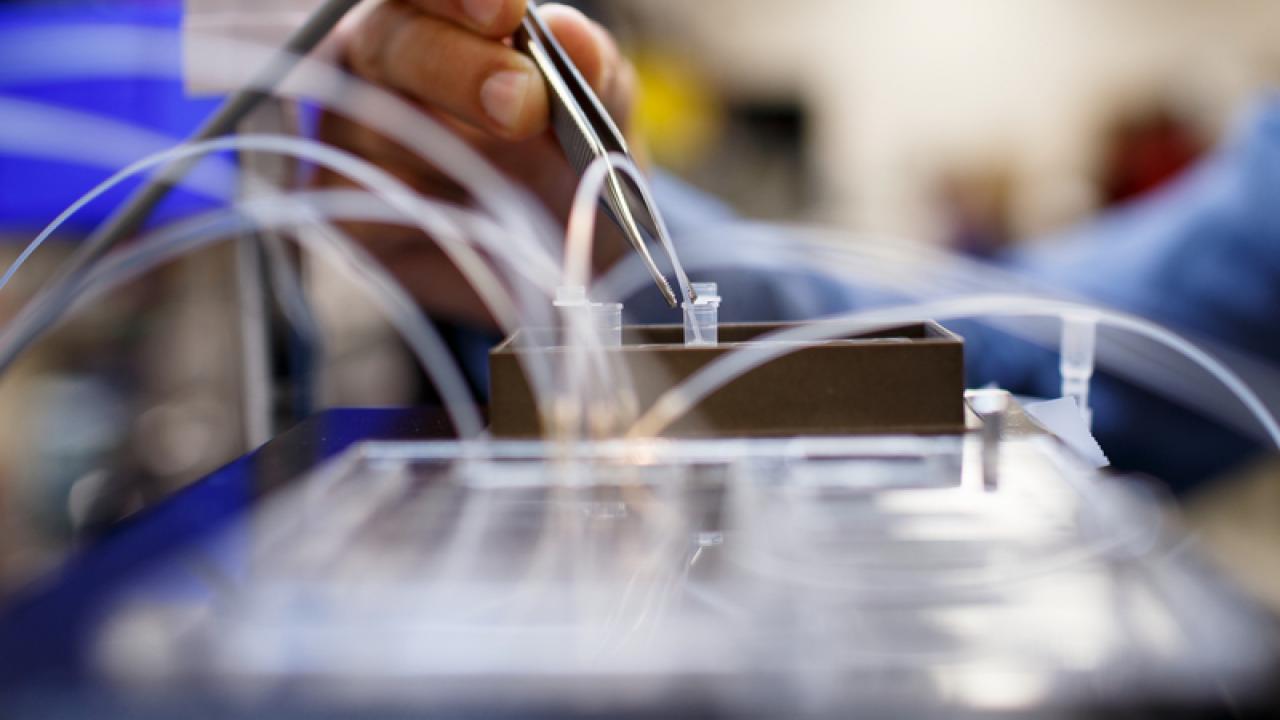
Photo by Steve Babuljak, 2015.
from UCSF Magazine Winter 2020
One morning, as you’re getting out of bed, an intense pain grips your feet. Your toe joints are swollen again. It’s been happening for months now. You decide it’s time to get the problem checked out, so you pay a visit to your doctor, who tells you that you have rheumatoid arthritis.
What happens next depends on who you are. If you’re white, for instance, with good health insurance and access to state-of-the-art care, your doctor probably doesn’t think twice before ordering a biopsy of your joint tissue and then sending the sample off for genetic testing. As luck would have it, according to the results, you’re a perfect match for a powerful new therapy. It’s woefully expensive, but luckily again, your insurance covers it. Within days, your pain and swelling are gone.
But what if you’re poor and uninsured? Even if you manage to cobble together enough money to pay for a genetic test out of pocket, there’s no way you can afford the recommended treatment. Or say you’re a person of color. Because researchers haven’t studied many people like you, no special therapy exists that targets your disease’s particular genetic profile. So your doctor prescribes the standard regimen of steroids and painkillers, which causes weight gain and puts you at risk for stomach ulcers. Plus, your feet still hurt.
Hala Borno, MD, oncologist and assistant professor of medicine at the UCSF Helen Diller Family Comprehensive Cancer Center.
This future scenario is, of course, hypothetical. But it reveals both the promise and the potential pitfalls of what’s known as precision medicine.
A revolutionary approach to patient care, precision medicine uses advanced biomedical tools, including genetic and molecular testing and big-data analytics, to help clinicians better predict which treatment and prevention strategies will work best for which patients. It aims to replace the current one-size-fits-all model – in which therapies and interventions are developed for the “average” person – with one that tailors care to each patient’s unique biology and life circumstances, including their race, finances, and living environment.