
UCSF Organizer Lewis Lanier introduces Abramson Cancer Center immunotherapy pioneer and symposium keynote speaker Carl June at UCSF Helen Diller Family Cancer Center Symposium 2015.
In closing the 2015 UCSF Helen Diller Family Comprehensive Cancer Center Symposium, President Alan Ashworth, PhD, FRS, counted himself among those who might once have underappreciated the full potential of cancer immunotherapy.
“But,” he declared, “it is clearly a field whose day has come.”
He also joined a few of the day’s speakers in noting that what feel like breakthroughs to outsiders have in reality been a 25-30 year evolution beginning to bear remarkable fruit and stoking a rare level of excitement in the cancer community.
Lewis Lanier, PhD and chair of the Department of Microbiology and Immunology at UCSF opened the day by using “cancer immunotherapy” and “cure” in the same sentence. Having dedicated his career to harnessing the body’s immune system against disease, Lanier marveled at the all-star teams assembled that day and the work they had accomplished to date.
 Other evidence came in lighthearted references to how at previous cancer meetings immunologists generally spoke in nearly empty rooms. Recently, however, such talks have been standing room only. Cole Hall was packed to the gills, with an overflow room to view the proceedings.
Other evidence came in lighthearted references to how at previous cancer meetings immunologists generally spoke in nearly empty rooms. Recently, however, such talks have been standing room only. Cole Hall was packed to the gills, with an overflow room to view the proceedings.
But the most compelling evidence was the work described by a who’s who of cancer immunotherapy.
These national and international leaders described building on trials that are beginning to demonstrate durable response in multiple cancer types. While displaying head-spinning images of T cells infiltrating and shrinking tumors, they spoke of next generation-type challenges: addressing adaptive response, resistance or side effects; finding new and creative ways to better deliver the powerful therapies; generating immune responses in one tumor locale to foster tumor repression and shrinkage in other parts of the body, and; becoming more adept at matching the therapies to not just disease types but to each patient’s unique biology.
The descriptions held the room rapt. Even among a group of cancer scientists who have good reason to feel caution about initial results, the excitement was palpable.
“Our day has come,” said Lanier, speaking in the days after the symposium. “In the past, with cancers, you had to cut ‘em, burn ‘em or poison ‘em. Now we can use the immune system to attack them and do so effectively.”
He adds, however, that while the successes are exciting, “Right now we have to hit the slot machine right; we can’t yet predict where immunotherapies will work.” He says next steps include better understanding the biomarkers, thinking beyond T cells, finding proper combinations so the cancers can’t mutate away and learning better which combinations of immunotherapies and, at times, chemotherapies are truly synergistic for which cancers.
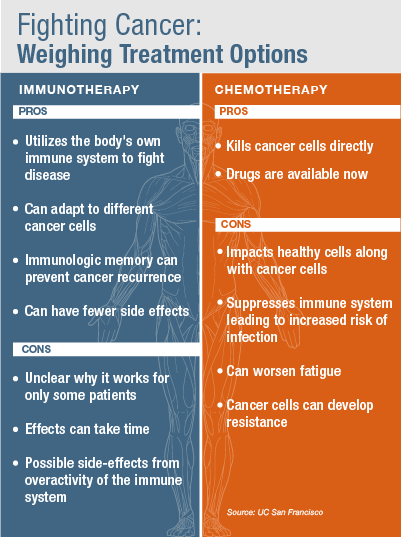
Lanier’s next steps fit well with Ashworth’s final comments, in which he made a plea for scientists to reject the false dichotomy between immunotherapy and chemotherapy, because advances in both fields may provide precisely the alliance needed to mount the next major leap forward. “There is just one camp,” he said, “people interested in curing cancer.”
The Talks
- Glenn Dranoff, MD, director of the Human Gene Transfer Laboratory Core at Dana Farber Cancer Institute who is moving on to a leadership role at Novartis: The Mechanisms of Protective Tumor Immunity
- Suzanne Topalian, MD, director of the melanoma program at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins: Immune Checkpoint Blockade: Mobilizing the Immune System to Treat Cancer
- Lawrence Fong, MD, and a genitourinary cancer specialist at UCSF Medical Center: Deciphering Human Responses to Immunotherapy
- Pamela Ohashi, PhD, FRSC and director of the immune therapy program of the Ontario Cancer Institute: Regulation of CD8 Immunity and Anti-Tumor Immunity
- Shannon Turley, PhD, and principal scientist for cancer immunology at Genentech: Stromal Cell Regulation of Immunity
- Matthew Krummel, PhD, faculty director of the Biological Imaging Development Center at UCSF: Visualizing Immune Deviation in Tumor Microenvironments
- Darrell Irvine, PhD, professor of biological engineering and materials science & engineering: Engineering Anti-Tumor Therapy with “Hitchhiking Therapeutics.”
- Elizabeth Jaffee, MD, deputy director of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins: Emerging Strategies for the Immunotherapy of Pancreatic Cancer
- Crystal Mackall, MD, head of immunology section and chief of the pediatric oncology branch of the National Cancer Institute: Optimizing CAR T cell Therapy: Progress and Challenges
- Ronald Levy, MD, and professor and chief of the Division of Oncology at Stanford University: Treating the Tumor and Treating the Host
- Wendell Lim, PhD UCSF, Using Synthetic Biology to Reprogram the T Cell
- Carl H. June, MD, program director of translational research at the Abramson Family Cancer Research Institute: Updates in CAR T Cell Therapy for Cancer.