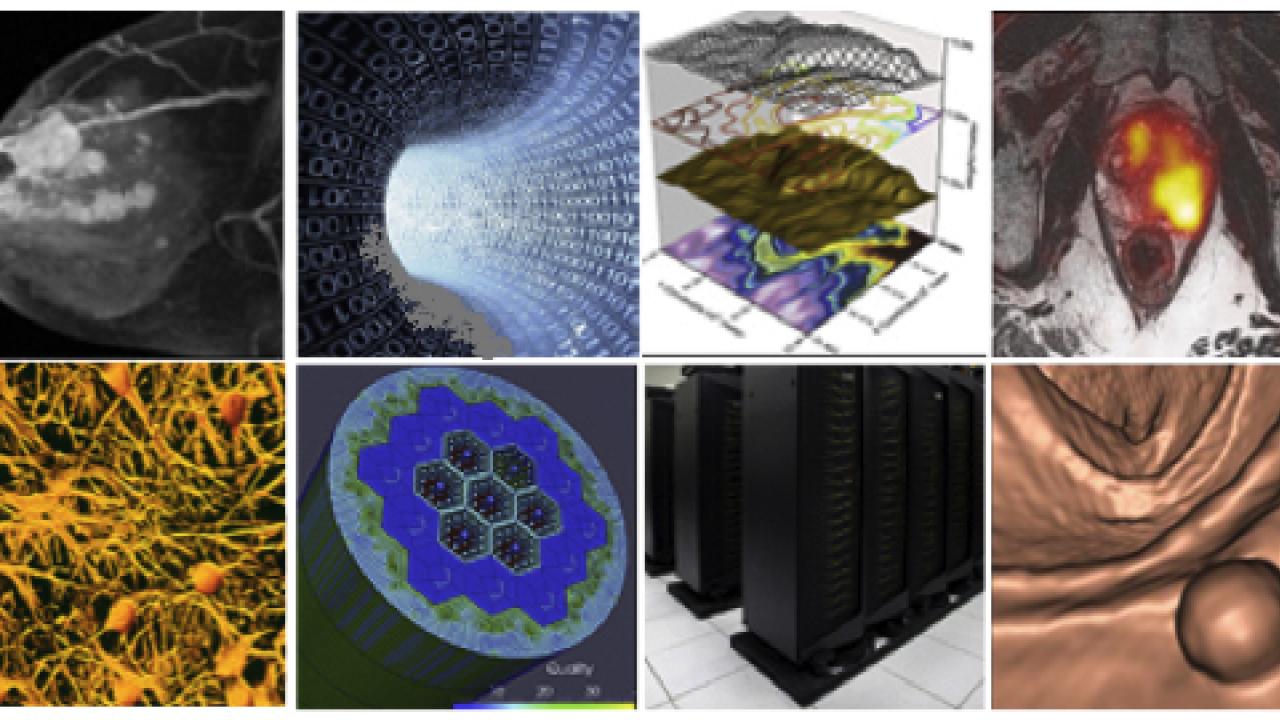
The Cancer Imaging Research Core aims to provide members of the HDFCCC with technical capabilities and scientific expertise for furthering their basic, translational, and clinical research using the latest imaging technology.
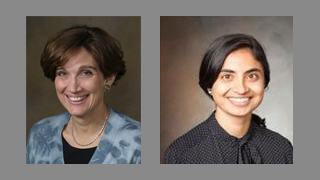 Scientific Director Sabrina Ronen, PhD (left), and Core Manager Emma Bahroos (right) took a moment to talk specifics about the range of services the core provides and how these can benefit the cancer research community at UCSF and beyond.
Scientific Director Sabrina Ronen, PhD (left), and Core Manager Emma Bahroos (right) took a moment to talk specifics about the range of services the core provides and how these can benefit the cancer research community at UCSF and beyond.
What is the purpose of your core?
The purpose of the Cancer Imaging Research (CIR) core is to provide technical capabilities and scientific expertise for integrating cutting-edge, multi-modality imaging into basic, translational, and clinical cancer research. We help potential users in designing, planning and executing the most appropriate imaging studies for answering their cancer research questions.
"Real time assessment of molecular changes in tumors by imaging in conjunction with anti cancer therapy are a vital need in the development of novel agents."
Dr. Pamela Munster
Director, Early Phase Clinical Trials Unit, Co-leader of the Center for BRCA Research, and Leader, Experimental Therapeutics Program, UCSF Helen Diller Family Comprehensive Cancer Center
What special technology or equipment does your core use that researchers find invaluable?
The CIR was only recently established. We welcome broad utilization of the wide range of scientific expertise and multi-modality imaging equipment available. The core provides imaging for anatomic, functional, and metabolic information and is organized into four groups.
- Pre-clinical imaging uses NMR/MRS, MRI, CT and PET/CT, radioisotope synthesis and DNP hyperpolarization systems.
- Human research uses MRI, PET/MR, MEG, Spinlab, hyperpolarized C-13 agent preparation, nuclear medicine tracer preparation.
- Clinical research uses clinical scanners, cyclotron, PACS, radiologists, imaging research analysts.
- Imaging Computer Services use high performance computing, specialized software packages, storage and back-up.
Is your core available to others outside UCSF and if so, how does their use differ?
Recharge rates differ for users outside of UCSF.
How can users be sure that the core can address their scientific question?
If you have a question and are not sure how imaging tools can be utilized, we encourage submitting a feasibility form to ensure a consultation with an expert. Potential users will be connected with imaging specialists who will advise on the best approach. If necessary a small CIR-supported feasibility study can be performed prior to the full imaging study.
What are some examples of prominent projects your core has contributed to?
Linking imaging and genomic markers through image directed tissue samples:
In this project, tumor heterogeniety was studied using image-guided genomics in low-grade gliomas. An important component of this research has been the acquisition of image-directed tissue samples from patients at initial surgery and at the time of subsequent surgeries for suspected recurrence. These have confirmed that there is spatial and temporal evolution of the molecular characteristics of the tumor, and that a subset of patients who are being treated with temozolomide progress rapidly due to hypermutations that can be attributed to its mechanism of action.
- 1. Johnson BE, Mazor T, Hong C, Barnes M, Aihara K, McLean CY, Fouse SD, Yamamoto S, Ueda H, Tatsuno K, Asthana S, Jalbert LE, Nelson SJ, Bollen AW, Gustafson WC, Charron E, Weiss WA, Smirnov IV, Song JS, Olshen AB, Cha S, Zhao Y, Moore RA, Mungall AJ, Jones SJM, Hirst M, Marra MA, Saito N, Aburatani H, Mukasa A, Berger MS, Chang SM, Taylor BS, Costello JF. Mutational analysis reveals the origin and therapy-driven evolution of recurrent glioma. Science. 2014;343(6167):189-193. PubMed PMID: 24336570; PubMed Central PMCID: PMC3998672.
Development, validation and translation of new imaging technologies: :
Our core has helped with translating new imaging technologies to firstin- man to demonstrate how hyperpolarized 13C metabolic imaging could be used to evaluate patients with prostate cancer. Hyperpolarized methodology has been utilized for early evaluation of treatment effectiveness in human subjects and found that a reduction in the conversion of pyruvate to lactate is associated with response to therapy.
- 2. Nelson SJ, Kurhanewicz J, Vigneron DB, Larson PE, Harzstark AL, Ferrone M, van Criekinge M, Chang JW, Bok R, Park I, Reed G, Carvajal L, Small EJ, Munster P, Weinberg VK, Ardenkjaer-Larsen JH, Chen AP, Hurd RE, Odegardstuen LI, Robb FJ, Tropp J, Murray JA. Metabolic imaging of patients with prostate cancer using hyperpolarized [1-(1)(3)C]pyruvate. Sci Transl Med. 2013;5(198):198ra108. PubMed PMID: 23946197; PubMed Central PMCID: PMC4201045.
Mutations in the IDH1 gene are early events and are present in over 80% of patients with grade 2 and grade 3 glioma. This knowledge has sparked a great interest in developing non-invasive imaging methods for evaluating such tumors. Pre-clinical model systems results show that injecting hyperpolarized [1-¹³C]α-ketoglutarate and following its conversion to [1-¹³C]2-hydroxyglutarate using dynamic MR spectroscopy is a promising approach for identifying tumors with pathogenic IDH mutations noninvasively.
- 3. Chaumeil MM, Larson PE, Yoshihara HA, Danforth OM, Vigneron DB, Nelson SJ, Pieper RO, Phillips JJ, Ronen SM. Non-invasive in vivo assessment of IDH1 mutational status in glioma. Nat Commun. 2013;4:2429. PubMed PMID: 24019001; PubMed Central PMCID: PMC3908661.
Providing quantitative imaging end-points to the user in a timely fashion so that they can be included in patient care:
Our core has helped develop a software pipenline for interpreting multi-modal imaging data. MR spectroscopic imaging (MRSI) provides spatially-resolved metabolic information. When used with anatomical and functional imaging, it can help improve treatment planning and monitor treatment response. The evaluation and interpretation of MRSI data has been streamlined with SIVIC (Spectroscopic Imaging, Visualization, and Computing), a flexible UCSF developed, open-source software framework, providing a scanner-to-PACS workflow.
- 4. Crane J, Olson MP, Nelson SJ. SIVIC: Open-Source, Standards-Based Software for DICOM MR Spectroscopy Workflows. Int J Biomed Imaging. 2013; 2013:169526. PMID: 23970895; PMCID: PMC3732592.
For more information, visit the Cancer Imaging Research Core.