Cancer and the Immune System
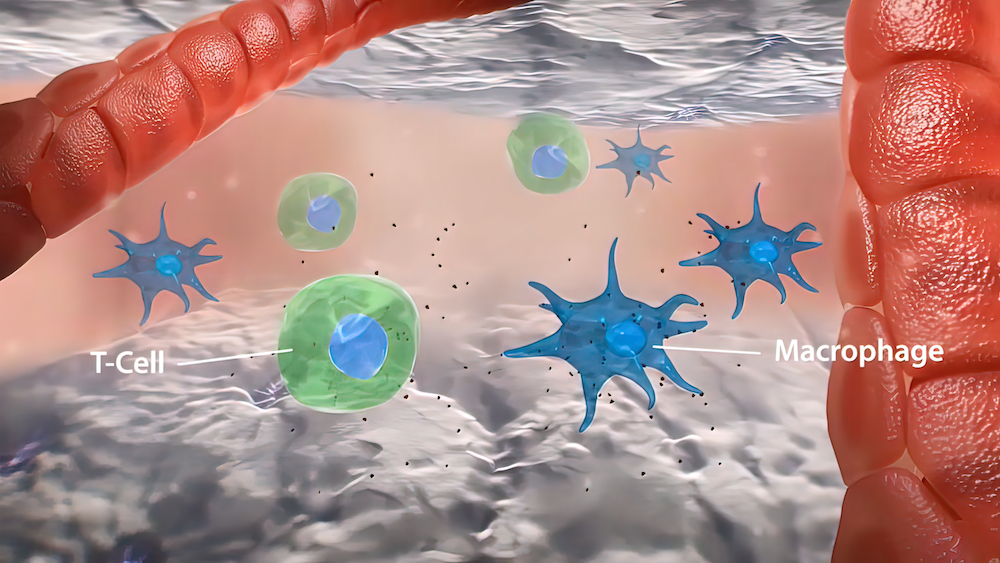
The immune system is a complex network of cells whose role is to defend the body against danger. These dangers include both infections and cancers. Just as the immune system is designed to recognize germs that may cause infection, it is also designed to recognize cells that have developed cancerous mutations. When potentially cancerous cells are identified, the immune system sends signals to specialized immune cells to seek out and to destroy them, thereby preventing cancer from occurring in the vast majority of cases.
Occasionally, however, cancerous cells evade detection by the immune system and are allowed to grow out of control. Sometimes this can occur because a person’s immune system is damaged, but most of the time cancer occurs in people with healthy immune systems. In these cases, the cancer cells are either too strong for the immune system to control, or have developed elaborate mechanisms to “hide” from the immune system.
Over the past several decades, researchers have identified many of the key cancer-fighting cells of the immune system as well as several of the ways that cancer cells are able to escape detection. This has paved the way for the field of cancer immunotherapy as a novel strategy to improve outcomes for patients with cancer.
What is Immunotherapy?
For more than half a century, the mainstay of cancer treatment has been chemotherapy. Traditional chemotherapy was developed from agents used in chemical warfare, and functions principally by damaging the DNA in cancer cells. Unfortunately, chemotherapy also damages the DNA in healthy cells, resulting in the typical side-effects associated with chemotherapy, including nausea, hair loss, and low blood counts. While traditional chemotherapy is effective for certain types of cancers, other cancers are able to survive even the strongest chemotherapy.
Immunotherapy is different than chemotherapy in that it harnesses the power of a patient’s own immune system. Immunotherapy can work by either “boosting” or by “re-training” a person’s immune system. Because cancers—much like infections—are due to malfunctions of the immune system, immunotherapy holds particular promise to help improve outcomes for patients with cancer.
The first example of a successful cancer immunotherapy was the development of bone marrow transplantation for blood cancers like leukemia and lymphoma. Bone marrow transplantation involves replacing a patient’s defective, cancerous bone marrow with the bone marrow from a healthy donor. Because the bone marrow contains important cancer-fighting immune cells, many patients are now able to be cured of cancers that otherwise would have been deadly.
In recent years, novel cancer immunotherapies have been developed that hold particular promise for potentially curing many other types of cancers. These include CAR T cells, checkpoint inhibitors, and cancer vaccines, among others.
CAR T Cells
T cells, or T lymphocytes, are one of the most important types of cancer-killing cells in our bodies. T cells have specific receptors that can recognize unique proteins on the surface of cancers, thereby allowing them to distinguish cancer cells from normal cells. Many cancers are able to grow out of control because they become resistant to the killing power of normal T lymphocytes.
Chimeric antigen receptor T cells, or CAR T cells, are T cells that are genetically modified to recognize specific proteins on the surface of cancer cells. Typically, a patient’s own T cells are collected, modified, and then re-infused like a simple blood transfusion.
The best-studied CAR T cells thus far are T cells that are genetically modified to recognize CD19, a protein which is found on the surface of most acute lymphoblastic leukemia (ALL) and lymphoma cells. For patients who have relapsed or refractory ALL, remission rates with conventional salvage chemotherapy treatments are 30% or less. With CAR T cell therapy for relapsed or refractory ALL, remission rates exceed 80%.
The UCSF Cancer Immunotherapy Program and Clinic are at the forefront of CAR T cell development, with clinical trials available for patients with leukemia, lymphoma, brain cancer, and pancreatic cancer. Over the next several years, we anticipate that CAR T cell therapy may become available for virtually all types of cancers.
Checkpoint Inhibitors
Immune cells in our bodies are trained to be able to distinguish dangers such as germs and cancer cells from our normal, healthy cells. When the immune system detects a danger, signals are sent for immune cells to rapidly proliferate in order to mount an attack. Once the danger is eliminated, other signals are sent in order to tell the immune cells to “stand down.” These signals are referred to as “checkpoints,” and help prevent autoimmune diseases that would result from an overly active immune system.
Many cancers are able to evade immune detection by sending similar “checkpoint” signals to the immune system telling it to “stand down.” In the presence of these signals, the immune system fails to recognize the cancerous cells as dangerous and allows them to grow out of control.
Recently, multiple checkpoint inhibitors have been developed that block these signals from cancer cells, allowing the immune system to recognize them as dangerous and to more efficiently kill them. Checkpoint inhibitors have dramatically changed the way that skin cancers, lung cancers, and urinary cancers—among others—are treated.
At the UCSF Cancer Immunotherapy Program and Clinic, we are studying novel combinations of checkpoint inhibitors and learning how best to use these agents in a wide range of cancer types.
Cancer Vaccines
Vaccines have long been used to help prevent infections. Vaccines work by exposing the immune system to a small amount of harmless proteins that are not normally found in the body. By exposing the immune system to these proteins in small amounts, the immune system becomes “trained” to recognize these as dangerous before a real threat occurs. They can also be used to “boost” the immune response even if an exposure has already occurred.
Similarly, cancer vaccines boost the immune system’s ability to recognize and to destroy cancer cells. There are several cancer vaccines that have already been FDA-approved, including vaccines to prevent cervical cancer and to help treat prostate cancer, but many more are in development.
At the UCSF Cancer Immunotherapy Program and Clinic, we are studying novel cancer vaccines both to prevent and to treat a wide variety of cancers.