 This information is given to provide you with an understanding of the procedures you will experience with the removal of your sentinel lymph node(s) or, the first lymph node(s) in the chain of lymph nodes under your arm. The sentinel lymph node(s), is (are) believed to most likely contain disease if the cancer has spread from the breast to the lymph nodes. Sentinel lymph node biopsy has been developed to decrease the potential complications of removing multiple lymph nodes from your armpit and to study those lymph nodes more thoroughly. Based on scientific evaluation of removing and testing fewer lymph nodes during breast cancer surgery, sentinel lymph node dissection is now an accepted and safe part of care. You may be asked to participate in a clinical trial.
This information is given to provide you with an understanding of the procedures you will experience with the removal of your sentinel lymph node(s) or, the first lymph node(s) in the chain of lymph nodes under your arm. The sentinel lymph node(s), is (are) believed to most likely contain disease if the cancer has spread from the breast to the lymph nodes. Sentinel lymph node biopsy has been developed to decrease the potential complications of removing multiple lymph nodes from your armpit and to study those lymph nodes more thoroughly. Based on scientific evaluation of removing and testing fewer lymph nodes during breast cancer surgery, sentinel lymph node dissection is now an accepted and safe part of care. You may be asked to participate in a clinical trial.
There are several ways to locate the sentinel node: injection only, injection and a nuclear medicine scan called lymphoscintigraphy, and/or use of a blue dye. Your physician will discuss which procedures best match your situation.
Who is a candidate for this?
Most people with early stage breast cancer are eligible. The indications are changing and we have several clinical trials to improve how we use sentinel lymph node biopsy.
Pre-operative:
On the day of or the day before your surgery, you will report to your pre-registration area or to the Department of Nuclear Medicine. Please check for this location in materials given to you by the surgery scheduler.
Injection of technetium sulfur colloid to locate the sentinel lymph node:
If this is your first lymph node surgery, you are likely to need an injection only. The injection may either be given to you in the Department of Nuclear Medicine or in the pre-surgery area. This is a brief single injection. A nuclear medicine physician injects a small amount of radioactive material (technetium sulfur colloid) into the breast. The material moves through the breast's lymphatic channels into the lymph nodes in your armpit.
Nuclear medicine scan (lymphoscintigraphy):
The scan is done in the Department of Nuclear Medicine. The scan is most commonly used when you have had lymph nodes removed before. The technetium is injected and travels as above through the breast's lymphatic channels into the lymph nodes in your armpit. During the procedure, which takes about one hour, you will be lying on your back on an exam table; a large camera will be moved around your body, and a technician will make images. The amount of radiation exposure with this procedure will be less than that of a routine chest x-ray.
The side effects associated with the injection or injection and scan include: pain at the injection site during and shortly after injection, possible redness and tenderness at the injection site lasting 1-2 days, and rarely, infection.
The injection or injection and scan determine the location of the regional lymph node(s) in your armpit most at risk for containing cancer cells. These are "locator" procedures and do not tell you whether or not the lymph nodes contain cancer cells.
Blue Dye mapping during surgery:
Rarely, if the injection of technetium does not find the sentinel lymph node, the surgeon injects a blue dye in the operating room. The blue dye is picked up by the lymphatic vessels and travels to the sentinel node(s). The blue dye may discolor (a blue tinge) the injected skin, the lymphatic channels, and the urine. If the discolored skin is not completely removed surgically, the blue color will remain for several weeks (sometimes months). The urine will return to normal color in 2-3 days. There is a possibility of allergic reaction to the blue dye at the time of injection, but this is rare.
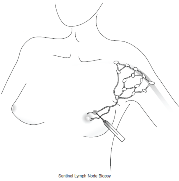
Locating and removing lymph nodes during surgery:
While you are in the Operating Room, readings will be done with a device called a Neoprobe (gamma counter), by placing a metal probe on specific areas of your skin, over the area of your breast cancer, as well as the lymph node(s) in your armpits. The machine then records numbers measuring the radioactive material (the technetium sulfur colloid injected in Nuclear Medicine), and assists the surgeon in locating the lymph node(s) to be sampled during the operation. The sentinel lymph node(s) are sent to pathology to be examined. you may have additional lymph nodes removed depending on your prior treatment, your clinical situation and your surgeon's recommendation.
