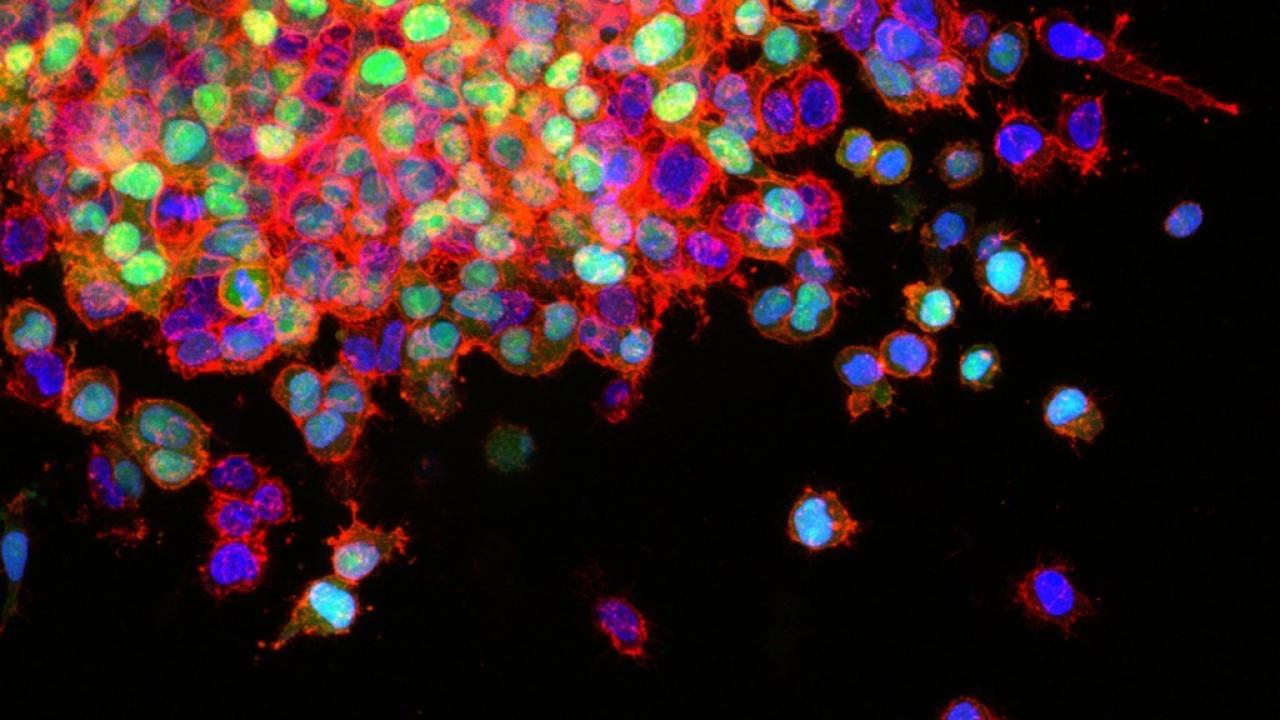
Lung cancer cells invading surrounding tissues and start to spread. Image courtesy National Cancer Institute.
The ability of lung tumor cells to spread rapidly within the body makes lung cancer difficult to eradicate and contributes to its status as the leading cause of U.S. cancer deaths in both men and women. But according to a new study led by UC San Francisco scientists, the cancer’s ability to spread may often be due to the inactivation of a single protective protein within tumor cells.
The researchers found genetic mutations in the protective protein, called Capicua (CIC), with disproportionate frequency in human lung cancers that have spread to other body sites — an event called metastasis.
Furthermore, the researchers determined that the protein could also be inactivated as a downstream consequence of common biochemical abnormalities that arise in lung cancer, even in cases where the CIC gene itself is not mutated. Some of these abnormalities, thought to drive tumor growth, are already being targeted by both FDA-approved and experimental drugs in clinical trials.
The new findings, published online November 21, 2016 in Nature Genetics, point to the possibility of reactivating CIC to stop the spread of lung cancer, said senior study author Trever Bivona, MD, PhD, associate professor of hematology and oncology and member of the UCSF Helen Diller Family Comprehensive Cancer Center.
“We found that this protein, first discovered as a regulator of development in the fruit fly, and also known to direct normal development of air sacs in the lungs, can be co-opted by tumors and inactivated to cause cancers to spread,” Bivona said. “While there are already treatments in development that might reactivate CIC and stop metastasis, more work is needed to reveal whether such a strategy will be effective.”
The study, a collaborative effort involving scientists from several research institutions in addition to UCSF, focused on the most common lung cancer, called non-small cell lung cancer (NSCLC), the most deadly form of cancer worldwide.
Most of the laboratory experiments were conducted by the study’s first author, Ross Okimoto, MD, a UCSF medical oncologist, who took the unusual and difficult step of injecting fluorescently labeled human lung tumor cells directly into the lungs of mice used to model the disease, instead of beneath the skin or into the tail vein, as is more typical.
Using gene sequencing on three closely related human lung cancer cell lines, Okimoto determined that there were few genetic differences between two metastatic tumor cell lines and a closely related but localized tumor cell line. This work quickly led to the identification of CIC gene deletion and lack of the corresponding CIC protein as a suspect in lung cancer metastasis.
Okimoto then monitored the metastatic potential of lung tumors in the mice by tracking fluorescently labeled tumor cells as they escaped from the lung and entered the bloodstream. He found that genetically engineering tumor cells to equip them with normal CIC gene resulted in the loss of tumors’ ability to spread.
The researchers then analyzed genetic data from hundreds of human lung cancers and found that CIC was mutated in metastatic lung cancer seven times more often than in lung tumors that had not yet spread. The same gene also is often mutated in metastatic gastric cancers, they discovered.