
Using a divide and conquer strategy, researchers from the University of California San Francisco have provided a road map for the development of a precision medicine approach to osteosarcoma, the most common bone cancer in children and young adults and an aggressive disease for which treatment has remained unchanged for more than 30 years.
Because osteosarcoma is complex and heterogeneous, lacking the disease-driving genetic mutations that could be targeted with therapies, the UCSF team identified other genetic characteristics that could be used to create subsets of the cancer, each of which then responded to a different targeted therapy.
The research, published in Cancer Discovery, “has fueled excitement in the patient community because there has been little progress in developing new therapies for osteosarcoma for decades and this gives people a handle on a path forward through subclassification and for biomarker-informed clinical trials,” said E. Alejandro Sweet-Cordero, MD, the lead author of the study and director of the Molecular Oncology Initiative at the UCSF Helen Diller Family Comprehensive Cancer Center.
An estimated 800 to 900 new cases of osteosarcoma are diagnosed every year in the United States. Current treatment entails surgical resections and the same standard multi-drug therapy for all patients, even though the drugs don’t work for all patients. Both options that have significant short- and long-term toxicities and morbidity.
For patients diagnosed with metastatic disease, or those who have relapse, the five-year survival rate is below 30 percent. In addition, an international, open-label clinical trial, published in Lancet Oncology in 2016, failed to increase survival outcomes by intensifying chemotherapy for high-risk groups.
Genetic sequencing, now relatively inexpensive and increasingly common, has fueled great hope in the oncology community because it has aided in the discovery of cancer-driving genetic mutations and led to the development of new therapies that target them. Unfortunately, this approach has so far been unsuccessful in osteosarcoma because it lacks significant mutations in protein-coding genes, said Sweet-Cordero, an associate professor of pediatrics at UCSF.
However, the UCSF team saw other genetic irregularities in osteosarcoma that were worth exploring for vulnerabilities. Osteosarcoma accumulates multiple copies of genes, sometimes as many as eight, 12 or more, rather than the normal two copies, Sweet-Cordero said.
One of the challenges in addressing osteosarcoma is that it has “a hopelessly complex genome and there’s not one genetic pattern,” Sweet-Cordero said. “It’s often described as a snowflake because every case is unique.” As a result, it’s hard to know what SCNAs are the drivers of the disease.
To get a clearer view of the breadth of SCNA in osteosarcoma, the UCSF team sequenced the whole genome and RNA of multiple tumors at different stages of disease and combined that information with public data on other sequenced tumors, he said.
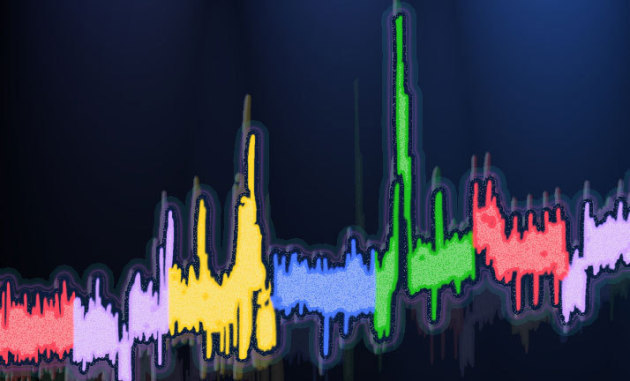
Genomic analysis of osteosarcoma (OS) and identification of recurrent SCNAs in primary tumors. Image courtesy Sweet-Cordero Lab, UCSF.
The UCSF team chose to focus on genes previously identified in public data as clinically actionable, meaning a drug was available to target it. Researchers used the presence of the SCNA in these driver genes to divide the cancer into subgroups. In cases with SCNA in multiple genes, they grouped the cancer based on the gene that was amplified the most.
Another major hurdle to developing new and improved therapies for osteosarcoma is the lack of reliable disease models. The team overcame this issue by creating xenograft mouse models using tissue originating from initial biopsies, post chemotherapy resections and metastasis, representing the full spectrum of the disease and its diversity. Testing verified the models had the same SCNA and gene amplification as the original patient-derived tissue samples.
The team identified potential therapeutic targets in the models by focusing on the SCNAs found in the same list of relevant driver genes that were used to break the samples into subsets. The team then identified the individual drugs that offered the most promise and treated each subset with one drug, rather than combination therapy commonly used with patients, to observe the target-specific effect of each drug. Some of the drugs were FDA approved, and others were tool compounds being used in the lab or tested in Phase 1 clinical trials, Sweet-Cordero said.
Each subset demonstrated statistically significant tumor reduction. However, it is important to note that no single drug was universally beneficial to all samples, highlighting the importance for matched, targeted therapies based on SCNA.
The results indicate that although osteosarcoma is highly heterogeneous, targeting SCNAs represents a potentially novel avenue to define patient-specific therapies for the disease. It also highlights how genome sequencing could help identify biomarkers that can be used to stratify patients into different groups for treatment with different drug combinations.
“By focusing on potentially actionable genes, we were able to reduce the complexity of the genomic landscape of osteosarcoma to identify alternations most likely to be of direct clinical relevance,” Sweet-Cordero wrote. “We expect that the next stage to advance genome-informed therapy will be the rational design of combination therapies, potentially with multiple targeted agents or a single targeted agent in concert with cytotoxic chemotherapy.”
Related links
