The new watchword for the frontlines of cancer treatment is “precision.” Whether here at the University of California, San Francisco or other leading centers around the world, the field’s best minds are probing more deeply than ever into the cellular and molecular underpinnings of cancer, and working to harness vast amounts of new data to revolutionize everything from diagnosis to the most effective drugs and the costs of care.
"One way to think about precision cancer medicine – and this new building designed in every way around the needs of patients – is that technologic and scientific advances over the past 15 years have led to an unprecedented understanding of cancer and what can be done about it."
Alan Ashworth, PhD, FRS
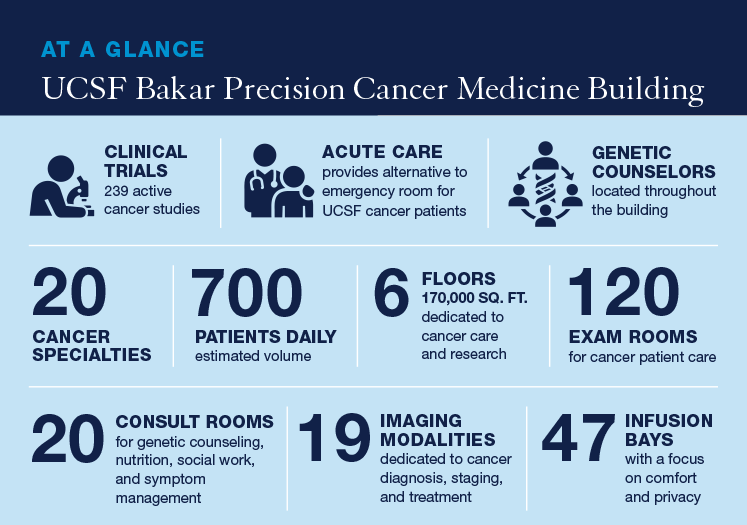
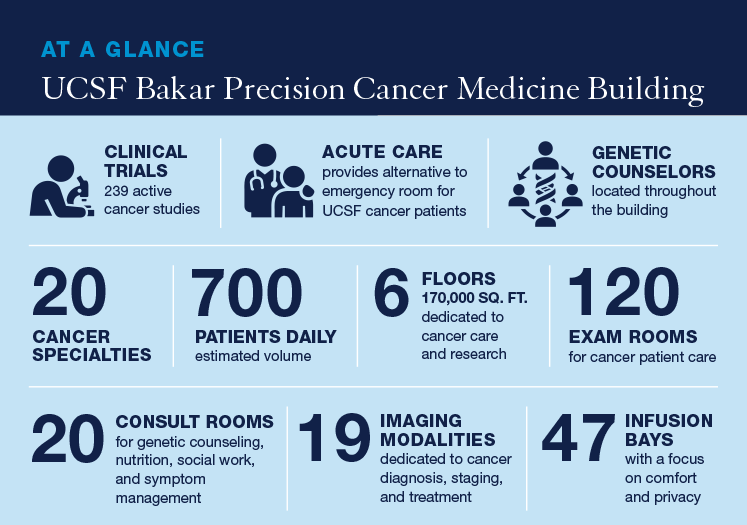
 Learn more about the UCSF Bakar Precision Cancer Medicine Building
Learn more about the UCSF Bakar Precision Cancer Medicine Building
The phrase “the right drug, for the right patient, at the right time,” in vogue a few years ago, doesn’t begin to cover the complexity of the terrain known as precision cancer medicine. Genetically-directed therapies are making new treatments possible. Extremely detailed analysis via tumor sequencing can find biomarkers that help unlock the secret to people’s cancer. Computer scientists are able to conduct complex analyses of massive data sets. Rapid advances in immunotherapy are turning the body’s defenses against cancer.
Despite all of this, many consider the field to be in its infancy but moving astonishingly fast. A symbol of this trajectory is the new
UCSF Bakar Precision Cancer Medicine Building which opened this week in Mission Bay. The treatments, technologies, and models of care offered to patients in this new space will reflect the most current thinking in how to tailor treatment to individual patients based on unique and defining characteristics of their tumors, personal genetics, and lifestyle.
This new center, the first of its kind in the Bay Area, represents where cancer treatment is headed.
“We’re moving to this age of much more refined and much more effective treatments,” says
Alan Ashworth, PhD, FRS, president of the UCSF Helen Diller Family Comprehensive Cancer Center. Ashworth is a pioneering scientist who co-discovered a way to kill BRCA1- and 2-related tumor cells by treating them with a class of drugs called PARP inhibitors.
The newest drugs, "don’t work on just anybody’s tumors," Ashworth says. "They were never designed to work on tumors generally, but rather on tumors that have a particular defect. This is at the heart of precision medicine."
Alan Ashworth, PhD, FRS, and Pamela Munster, MD, established the Center for BRCA Research, one of only two such centers in the US.
Pamela Munster, MD, is a breast oncologist with unique insight into the science of precision medicine and how it reaches the patient. She is a cancer survivor with a BRCA mutation who leads the cancer center’s experimental therapeutics program and co-founded with Ashworth the Center for BRCA Research at UCSF.
“As a clinician, I have had the opportunities to weigh in and collaborate with many scientists who have new strategies, new compounds and new products and then get them into the clinic,” Munster says. As a scientist, she says, “at the same time, I work with clinicians in terms of where to take a drug that looks promising, and how do you find biomarkers?”
With her leadership in early phase clinical trials and experimental therapies, Munster helps her fellow clinicians “select patients who are more likely to benefit.”
In the Service of Patients

Hani Goodarzi, PhD
The definition of precision medicine is anything but precise. Researchers and clinicians vary on what makes it work. Just like the science, the phrase itself is still evolving as it stands on the cutting edge of modern medicine.
Hani Goodarzi, PhD, an assistant professor of biophysics and biochemistry, brings both a biological and a data science background to the field. He doesn’t think of “precision” in the way one might imagine, of a scalpel or a laser carving out cancer.
“It’s not that it’s making anything precise in the sense of developing tools that act precisely,” he says. “It’s the fact that we can integrate a lot more information than we could historically to inform the decision-making process in health care.”
To
Atul Butte, MD, PhD, a world-renowned expert in medical technology who leads UCSF’s Institute for Computational Health Sciences, precision medicine brings many disciplines together in the service of patients—from biology and genomics, to the population science buried in electronic health records, to data an individual might generate on a smartphone or Fitbit.
“Precision medicine is the customization of medical care that we to deliver to a patient, based on measurements from that patient,” Butte says. “Certainly, they’re going to be biological measurements like DNA, proteins and things. But I think we’re also going to need behavioral measurements. I might need to get to your lifestyle. I might get some of those from your phone or from your wearables.”
“I certainly need to ask you your preferences: ‘I can tolerate this kind of side effect. I don’t like that kind of side effect,’” he says. “That’s also a part of precision medicine.”
Butte, who is also the chief data scientist for the UC Health system, bringing together five hospitals across California, says that data—when treated respectfully and safely—can yield tremendous insights.
Butte came to UCSF in 2015 in part for the opportunity to work with the massive UC system, which sees 16 percent of all cancer patients in the state. Also, because UCSF is in many ways one of the founding institutions of precision medicine. UCSF helped the National Institutes of Health launch a landmark precision medicine effort in 2011, putting the term on the map.
To Butte, the age of precision medicine has arrived and is only getting better.
UCSF is in many ways one of the founding institutions of precision medicine. UCSF helped the National Academy of Sciences launch a landmark precision medicine effort in 2011, putting the term on the map.
Winning at Whack-a-Mole
Alan Venook, MD, the associate director for program development at UCSF’s Cancer Center, goes one step further, asserting that the term precision medicine—at least as applied to cancer—is aspirational, a statement more reflecting where things are heading.
“No self-respecting cancer is just going to be able to be targeted with one drug,” Venook says. “It’s like a whack-a-mole. You block one process in the cancer and something else will take over.”
To be sure, cancer is a formidable foe. When it takes hold in a person, bad cells multiply and metastasize. They often develop resistance to the many ingenious methods devised to fight them.
For all the advances, all the years and billions of dollars spent, much of it remains a mystery. Cancer is still often a stone-cold killer indiscriminately taking lives.
That’s why Ashworth talks unabashedly, about a cure.
“I think we should be aspiring to cure and saying ‘cure’ much more than we do in what we want to ultimately achieve,” he says. “I think it’s defeatist to think otherwise. People talk about making cancer into a chronic disease, like diabetes. Although a laudable medium term goal, I think that’s a failure of long-term ambition.”
As an example, Ashworth cites advances once dismissed as impossible.
“Stage four melanoma was almost invariably lethal, and yet now a significant minority of patients appear to be long term survivors who may well be cured,” Ashworth says. “That came about because of immunotherapy, and most people didn’t see that coming. “Maybe a cancer very hard to treat, and it may be currently incurable, but that doesn’t mean it’s always incurable,” he says.
“Bespoke” Treatments
The immunotherapy of which Ashworth speaks is a prime example.
Lawrence Fong, MD, who leads UCSF’s Cancer Immunotherapy Program, says that in the past seven years, “cancer immunotherapy has become one of the mainstay approaches for treating cancer now.”
Prior to that, Fong says, “we typically used either chemotherapy, radiation therapy, or targeted therapies—drugs that hit mutations as means for cancer treatment. Those are treatments that we felt would directly kill cancer cells. But what immunotherapy does is it actually relies on the patient’s own immune system to kill the cancer cells.”

UCSF's Dr. Lawrence Fong speaks at the 2019 Precision Medicine World Conference in Santa Clara, California. Photo by Noah Berger
“We now have that in the form of antibody treatments that serve to turn on a patient’s immune system response,” he says, “and we also have that in the form of cell therapies where we can actually engineer cells from a patient to go after the cancer cells.”
Fong marvels at how far immunotherapy has come in such a short time. It is now a frontline therapy for major diseases like lung cancer; it is now enough of a “standard of care” that first year medical students are learning about it. “I would never have predicted it would be used for as many cancers as it is now,” he says.
Fong imagines where the field is headed as researchers pursue a Holy Grail of looking at people’s genetics, their immune system, and other factors and developing a “bespoke cancer therapy that integrates different elements that we think would be required for a successful outcome.”
A Patient-Focused Approach
Cancer’s extreme heterogeneity – that it may be several hundred different diseases – has been its best defense against more of the cures that Ashworth and Fong talk about. But on this new frontier of cancer research and treatment, things are changing.
“One way to think about precision cancer medicine – and this new building designed in every way around the needs of patients – is that technologic and scientific advances over the past 15 years have led to an unprecedented understanding of cancer and what can be done about it,” Ashworth says. “As we work toward more cures for more types of cancer, this new understanding means that UCSF can offer patients a level of care that is specific to them as individuals and informed by the most current thinking. UCSF has made a significant contribution to this thinking.”