
The Community Advisory Board of the Helen Diller Family Comprehensive Cancer Center in 2018.
Over the past 15 years, the cancer center’s Community Advisory Board (CAB) has become one of UCSF’s most instrumental community outreach groups for improving health equity. In a Q&A below, CAB Chair Arnold Perkins and Dr. Kim Rhoads discuss why CABs are critical to the work of NCI cancer centers and the communities they serve.
Q. Let’s begin with the obvious question. What is the role of CABs in cancer centers and who comprises membership?
Rhoads: Over the past decade, the National Cancer Institute has increasingly emphasized the importance of community engagement to inform the content and approach to cancer research conducted by investigators in comprehensive cancer centers. Community advisory boards are often convened in circumstances like this, when multi-stakeholder inputs are needed. That said, the Community Advisory Board for our cancer center was established long before the NCI elevated the importance of community engagement. CABs can be comprised of a variety of stakeholders. Our CAB includes representatives from community based organizations, faith community members and community advocates from across the Greater Bay Area; all of whom are engaged in ongoing work to increase health equity and reduce health disparities. Our CAB aims to ensure that our institution has year-round, non-transactional community engagement; that equitable academic-community partnerships are facilitated and that cutting edge cancer information is disseminated to the community.
Arnold Perkins
Perkins: The CAB is an opportunity for the academic community and the community at large to come together to talk about both cancer prevention and treatment. It’s so important that we are able to put the academic language into common everyday language, and that’s part of the role of the CAB. The CAB is comprised of members of various communities that are impacted by cancer. Our CAB covers a wide range of communities, from regions as far north as Eureka and as far south as Santa Clara.
Q. CABs began emerging about 20 years ago, and although the National Cancer Institute does not require that cancer centers have them, they are considered critical and are tacitly expected. Why should academic cancer centers have CABs?
Rhoads: While they may be tacitly expected by NCI, I don’t think having a CAB in order to check off a pre-requisite can achieve the true goals of community engagement in cancer. The point of having a CAB is to influence the research of the center. This means that the center needs to have the capacity to respond to the concerns voiced by; and needs expressed by the CAB. These needs and concerns must not only be heard, but also understood and translated into community level action. Those actions typically involve the promotion of cancer screening and early detection, but can also address the need for access to cancer information (for those who are diagnosed) and cancer treatment. The CAB members provide a link to larger community networks of people that we might not otherwise be able to reach. The links to these communities help our cancer center tailor ways to intervene on cancer disparities.
Perkins: Because they are the link to the community for the academic environment, the CAB is the voice of the community to the academic institution. It is critical that we have community participants to give voice to and influence the research. We serve a role as interpreters. It’s called the community advisory board, so our role is to advise the cancer center on the issues we see occurring in the community. It’s a leveling opportunity.
Q. In 2005, Rena Pasick, DrPH, and professor emerita, Dept. of Medicine, established this CAB. The first chair was Frank E. Staggers, MD, a renowned and beloved urologist and community activist who died in 2013. Please talk about the vision that Drs. Pasick and Staggers brought, and how that vision informs the work of today’s CAB.
Rhoads: I only met Dr. Staggers, Sr. once in person. But to hear Dr. Pasick tell the history, Dr. Staggers was the true visionary behind the establishment of the CAB and the first committee—the Faith Communities Committee, led by Ms. Gloria Brown. Dr. Pasick should be commended for her responsiveness to the request from her community advisors. As I previously pointed out, UCSF was on the cutting edge of community engagement in cancer by developing a CAB and the Office of Community Engagement before NCI realized how important these structures would be to addressing disparities. The durable relationships that Drs. Pasick and Staggers developed have given our institution a huge advantage in our efforts to eliminate cancer disparities.
Perkins: I met Dr. Staggers when I was 19 years old. I was the head of the ward he was on and his surgical assistant in the operating room. He shaped my life and was an incredible visionary. His vision was to have a broad section of the community interact with UCSF because we had been two separate bastions that had not interacted much before. He felt that the university was always speaking for the community but wasn’t really involved in it. So he had the vision to get people from the community involved with the university. It has made the CAB much better over time. In the past, CABs had been put forth as a rubber stamp, and Dr. Staggers was not having any kind of rubber stamps! The vision was to be as inclusive as possible and to pull from various parts of the community to form the board. His vision of community involvement is still what motivates us today—the goal is to have the community ensconced in the university.
We should also mention Priscilla Banks too. She was like the glue that held us together. She brought the community to the table and so really it was a threesome. Dr. Staggers had the vision for community participation; Dr. Pasick had the academic credibility and understanding of the academic community; and Priscilla had the prowess to bring the community to the table and identify who in the community we should tap into.
Q. When you assumed your current leadership positions – Dr. Rhoads as faculty leader of the CAB via her role as associate director for Community Engagement in 2018; and Mr. Perkins as chair of the CAB in 2013 – what did you feel you were inheriting? And what did you consider were your primary obligations and objectives going forward?
Rhoads: When I joined the cancer center in 2018, I was coming from a clinical career in surgery, and the founding of the community engagement program for the Stanford Cancer Institute. The transition back to my academic home (I was a UCSF medical student, surgical resident, colorectal surgery and health policy fellow) was exciting. I was so honored to be invited by Dr. Pasick to follow her as the director of the Office of Community Engagement. She and Priscilla Banks had curated a powerful, active and engaged community advisory board. I felt a tremendous amount of pressure because of Dr. Pasick’s nationally recognized contributions to community engaged work, and at the same time, I had an overwhelming sense of excitement about how the infrastructure she had put in place could be leveraged to go even deeper in our engagement with community to address some of the inequities in cancer care that I had been writing papers about before I arrived. The potential was so exciting but also a bit overwhelming.
Perkins: At times, the community has felt that university could be more receptive and engaged. So, the CAB started looking at the different programs in the cancer center, understanding that we needed to be more specific in our cancer focus. Around this same time in 2015 and 2016, the San Francisco Cancer Initiative (SF CAN) was in nascent stages of development. We felt that we had the opportunity to tap into an outstanding person who understood medicine, research and more important community, and that was Dr. Kim Rhoads. We are now grounded in the community, closer to the community than we ever have been before. We are doing an array of things centered around cancer and COVID-19. We are more community-centric than we have been, and we have developed a better understanding of the role of the community within the university.
Q. In what ways do you think the CAB has been influential in the direction or mission of the cancer center?
Rhoads: The CAB has been influential in dictating the terms of community engagement. One of the traditional complaints from community organizations and advocates about cancer centers and other academic institutions is that when we develop projects that require community involvement, we often think about community last. The programs we now have in place provide opportunities to engage with community partners before projects are implemented. When we started providing these opportunities, we had to reach out to the investigators who largely had already developed their project ideas. Now, we have requests coming in from investigators. They want opportunities to get feedback on their study related materials and ideas and are increasingly looking for community to work collaboratively on project development. The CAB’s willingness to fully engage, ask challenging questions, and pose alternative approaches has been met with an openness to pivot and to integrate community members into select research teams with important and remarkable impacts.
Perkins: The CAB has been influential by developing and supporting SF CAN, Umoja Health COVID-19 testing the pop ups, and much closer ties with the community. We have influenced the cancer center leadership. I can call Alan Ashworth (President, UCSF Helen Diller Family Comprehensive Cancer Center and Senior Vice President for Cancer Services, UCSF Health) at any time and say this is what needs to happen. Other members can call him or Bob Hiatt (Associate Director of Population Sciences, and Co-Leader, Cancer Control Program, UCSF Helen Diller Family Comprehensive Cancer Center). There is a better working relationship, a more collegial relationship between the CAB and the center now.
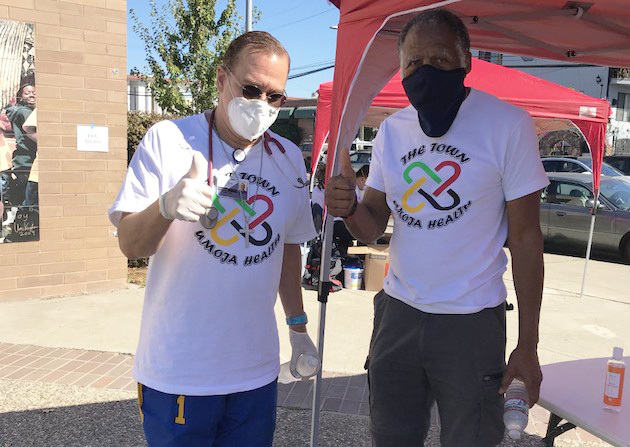
Arnold Perkins (right) at a recent Umoja Health Pop up with Dr. Geoffrey Watson.
Q. What would you cite as the CAB’s most significant achievements concerning the community?
Rhoads: In 2018, we became aware of the Patient & Family Advisory Council (PFAC). Laurel Bray-Hanin, vice president and chief operating officer for Cancer Services, observed that the advisory council was not as diverse as it could be and suggested that we consider how to integrate some of the activities of the CAB with the efforts of the PFAC. Keren Stronach, Patient and Family Experience Specialist, and I worked together to understand the PFAC and CAB roles and identify opportunities for synergy. We are both particularly proud of our first joint effort to improve patient care in the cancer center, jointly working to translate and culturally tailor the Cancer Patient’s Guidebook for patients with limited English language proficiency. Prior to that, the book was only available in English.

Members of the Community Advisory Board's Men's Health Committee (MHC)
I would also highlight the work of our Men’s Health Committee (MHC), led by Michael Shaw, the director of the Office of Urban Male Health at the Alameda County Public Health Department. The MHC leveraged their relationship with UCSF and their links to a large network of agencies in the East Bay to fuel what has become Umoja Health; a significant effort to increase COVID-19 awareness and testing in the African American community. The program has received praise from Chancellor Sam Hawgood as an example of our ability to develop equitable partnerships to address disparities during the pandemic.
Perkins: The work with the groups in Bayview Hunters Point around research on the environment and cancer; helping to open the Industry Documents Library, Bayview Hunters Point Collection is significant. Other activities with Rafiki Coalition for Health and Wellness; and with partners in the East Bay and Umoja Health are significant. The work with San Francisco Women’s Cancer Network, headed by CAB member Olivia Fe; Ysabel Duron’s work with the Latino Cancer Institute is also important. So much work has been influenced by the CAB as a body and its individual members. The Abundant Life Health Ministries Network, now led by Wilma Batiste, has reached thousands of folks with cancer information through a religious/faith based lens. That and the development of the MHC Friends of Frank committee are a direct tribute to the legacy of Dr. Frank Staggers, Sr.’s work. Our annual events put on by our CAB committees have been significant opportunities for the kind of community participation that Dr. Staggers envisioned.
Faith Leaders Preach Healthful Living UCSF.edu, Oct 2011
The Abundant Life Health Ministries Initiative is a partnership between UCSF and nearly 30 churches across the Bay Area to address health disparities of minority populations.
Q. A question for Mr. Perkins – have you seen a maturation in the relationship between the cancer center and the community as a result of the CAB’s guidance?
Perkins: Yes. As I mentioned before. We have been growing together over time. Dr. Staggers laid a strong foundation that we’ve been building on ever since. With a new staff in the cancer center’s Office of Community Engagement, we have been building within the community, and reaching out to multiple counties as far north as Eureka and as far South in Santa Clara.
However, we still have a lot more to do. We should be talking about developing centers of excellence; working closely with the UCSF Center for Community Engagement, and be in conversation with all the other CABs on campus so that UCSF has a more global approach to the work with community. There tend to be separate entities with interests in common, but we are unaware of them. We could be learning from what we have in common as well as the differences we have. So we are still growing and maturing.
Q. How has the charge of the CAB changed over the years, and what do those changes say about the focus on disparities, the direction of cancer research and treatment, or conditions in the Bay area?
Rhoads: The original charge from the NCI was that cancer centers are required to have a focus on community engaged efforts to address disparities in the defined catchment area. The NCI guidelines are evolving and now emphasize that the community-engaged work should be infused across the entire cancer center versus functioning like an appendage to the research agenda. This suggests an acknowledgment by NCI that the ways we have attempted to address disparities in the past, which were largely siloed efforts from basic and clinical research, are not having the positive impact they would like to see.
Perkins: The CAB’s charge started out to address health disparities. Then the CAB raised the importance of health inequity. The issue is that cancer disparities come from the inequities that also exist within the medical universe and the university. The community and university are often not on equal footing. We miss each other in our language. The university’s language is can be academic and hard to understand. We could be using simple language. Sometimes these basic questions are the most important question. We miss opportunities for successful exchange.
Q. Advances in cancer research and treatment are coming more rapidly than ever. How can the cancer center and the CAB navigate these changes to ensure that minorities and other underserved populations are comprehensively and ethically included in research, benefit from it, and are not further disenfranchised?
Rhoads: Advances in cancer research and treatment are recognized and celebrated inside the institution. That means that even if the advances are related to specific racial/ethnic groups, these groups don’t learn about these research findings. In other words, sometimes our discoveries are never known of or appreciated by the communities they are meant to impact. Our office has devised a way by which new technologies can be disseminated to the community. We will continue increasing community access to information and in the future will work to embed very intentional approaches to reducing inequities in our clinical cancer care delivery settings. To ensure that these advances reach diverse and underserved communities, we will eventually need to develop strong partnerships with oncology providers across the state. The community based oncologists serve the majority and most diverse group of patients with cancer.
Perkins: The center needs to aggressively reach out into the community with the latest cancer research vetted by organizations like the CAB. They should explain the latest advances and allow us to give input about where the most viable places and groups for this. I would like to see the CAB play a role in identifying where the disease burden can most effectively be treated. The Cancer Center and the university as a whole need to spend more time talking about advances for local community members, using the local media, TV, radio, etc. The advances are largely unknown. The people who can access that information are those with wealth and privilege. Others may not know. It will save money if we work harder to treat people in low resource communities early, otherwise we end up spending a lot of money in the subsequent treatment of more advanced cancers. We can save lives and save money too (with early detection and treatment). It’s an economic and human proposition. We know which communities have a high cancer burden, we have some sense of what that cancer burden is, so shame on us if we are not aggressively trying to reach and heal the people who need it.
Q. What will be the CAB’s priorities in the next five to ten years; and what would you like to see transpire between the CAB and the cancer center in that time?
Rhoads: Given the conditions in the larger society right now, with a poorly controlled global pandemic and economic indicators of high unemployment, increasing homelessness and food insecurity, our work will not be linear in the coming years. I suspect we will be addressing these issues in response to what our CAB and community partners are telling us are important to them. That said, I suspect we will be developing strategies to support people to get screened and if diagnosed, to finish treatment. This will be impacted by forced choices—for example, choosing between the cost of food and the cost of care, including screening as well as subsequent care. Activities like Umoja Health, which evolved directly out of our work with the Men’s Health Committee, are bringing together community organizations that normally provide support services in different domains of the social determinants of health (housing, education, employment, etc.). This is a practice run for what will be needed. The Umoja Health test sites are fertile ground for cancer information dissemination; and the Community Wellness Team, which provides community-led services for those who test COVID-19 positive. The model of taking health information and health services “to the streets” and to people’s homes is one model for how we can support the social determinants for community members facing a cancer journey. The more mundane answer to the question is that we hope to get better integration of our CAB and community partners in designing and implementing cancer research. In our Office of Community Engagement, as we facilitate these activities, we will be looking to promote projects that aim to have real world impact instead of projects that promise to deliver a high- impact publication.
Perkins: Going forward, we want to provide current and advanced cancer treatment to the least of us. We want to make sure that every person in our catchment area has the latest treatment available and we want to make sure the CAB partners with the cancer center to cause this to happen. The vital link has been the Office of Community Engagement. It is critical that the office reaches out into community to address the range of inequities that lead to cancer, including social stressors and begin paying attention to all of the factors that lead to families losing members. We have to be more diligent in looking at health overall and having cancer be a part of that. Sometimes we focus too much on cancer and don’t look at the environmental social economic factors that lead to cancer. It’s not just a biological disease, it has impacts on all aspects of and can be all-consuming in the family. I would love to see the cancer center become more familiar within communities that are struggling.
Separately, we should advocate for universal health coverage. We know that people with financial and educational means to negotiate and pay for treatment get the best outcomes. We want to see it become more equitable. We are such a wealthy country with such poor outcomes. The money we spend and the outcomes we get are not equitable. Health is a human right. Being a human being is to take care of our brother and sister, operating as one. That is what I would like to see us focus on.
In the News:
- Experts hope to fight COVID-19 vaccine distrust among Black community through education ABC7News, 12/20
- Oakland, Where Prostate Cancer and COVID-19 Intersect Oakland Voices, 12/20
- United in health: the quest to test Black residents for Covid-19 Mission Local, 11/20
- Agenda & Symposium Packet: 13th Annual “Gathering” Health Ministries Symposium for Faith, Health & Community cancer.ucsf.edu, 09/20
- Faith Leaders Preach Healthful Living UCSF.edu, 4/13
- Special event focuses on abundant life through faith, health & community UCSF.edu, 9/09
Links:
