
Hematology/Oncology Nursing

Katharina Ganapathi, RN
Clinical Practice Nurse

Jenner Wells, RN
Clinical Practice Nurse

Amyloidosis is a rare protein deposition disease where misfolded protein come together to form fibrils, deposit in the organs and cause organ dysfunction.

Clinical Practice Nurse

Clinical Practice Nurse
Amyloidosis is a rare protein deposition disease where misfolded protein come together to form fibrils, deposit in the organs and cause organ dysfunction. Under the microscope, the defining features of amyloid deposits include staining with a dye called Congo Red that renders apple-green birefringence under polarized light (Figure 1A and 1B). There are many different types of amyloidosis depending on what the misfolded protein is (Table 1). It is important to understand what type of amyloid is present in order to prescribe the correct treatment.
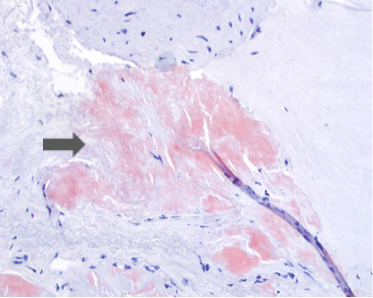
Figure 1A: Cardiac biopsy with Congo Red Stain on Light Microscopy. Amyloid (arrow) stains orange-red. Photo provided by Dr. Philip Ursell.
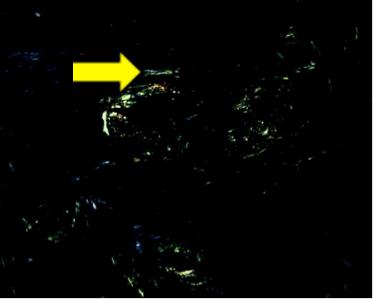
Figure 1B: Cardiac biopsy with Congo Red Stain under Polarized Light. The light green material (arrow) is amyloid. Photo provided by Dr. Philip Ursell.
Of the numerous types of amyloidosis (see Table 1), the most prevalent type is light chain amyloidosis (AL amyloidosis), in which approximately 4,500 new cases are diagnosed every year and the typical patient is between 50-80 years old. As with multiple myeloma, light chain amyloidosis is also disease of the plasma cells in the bone marrow. However, in AL amyloidosis, the plasma cells over-produce a misfolded version of the light chain part of an antibody molecule. These misfolded light chain proteins aggregate and are deposited in the organs of a patient’s body causing a range of symptoms.
Table 1: Types of Amyloidosis
| Type | Abbreviation | Clinical Manifestations |
|---|---|---|
|
Light chain |
AL |
May be localized or systemic. If systemic, common organs involved include heart and kidneys. |
| Wildtype transthyretin | ATTR-wildtype |
Older patients
Heart, soft tissue involvement (ex. carpal tunnel)
|
| Mutant transthyretin | ATTR-mutant |
Inherited/Familial
Heart, nerves, eyes involvement
|
| Serum amyloid A | AA |
Chronic inflammatory conditions
Kidneys, liver, nerves
|
| Beta-2-microglobulin | ABeta2m |
Long-term dialysis patients
Carpal tunnel syndrome, shoulder pain, and flexor tenosynovitis of hands
|
The signs and symptoms of this disease depend on which organs are involved. In light chain amyloidosis, the most commonly affected organs include the kidneys, heart, nervous system, and the gastrointestinal tract. AA amyloidosis most commonly affects the kidneys. In familial amyloidosis, the organs involved depend on the particular genetic mutation, but the most common are the nervous system and heart. Age-related amyloidosis primarily affects the heart.
Cardiac: In the heart amyloid deposits cause the heart muscle to become stiff (Figure 2). The heart muscle cannot function efficiently as a pump, resulting in heart failure. The patient may experience fatigue, shortness of breath, leg swelling or abdominal swelling. In addition, the amyloid deposits in the heart can interfere with the electrical activity of the heart, resulting in abnormal heart rhythms.
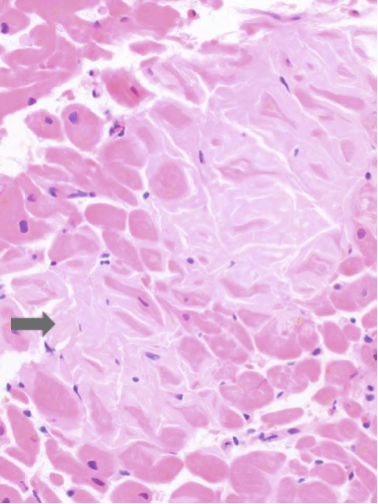
Figure 2: Cardiac biopsy with H&E stain. Between the muscle fibers, the light pink material (arrow) is amyloid. Photo provided by Dr. Philip Ursell.
Kidney: When amyloid builds up in the kidneys it is toxic to the small filters in this organ. The filters in the kidney become leaky and an essential blood protein called albumin leaks into the urine. Patients with early kidney amyloid may not have symptoms but later may develop foamy urine. Low albumin in the blood leads to swelling of the ankles. Some patients may go on to develop kidney failure.
Nervous system: Deposition of amyloid fibrils into the nervous system causes damage to nerves, a condition known as neuropathy. The exact symptoms depend on the nerves involved. If amyloid affects the long nerves that exit the spinal cord, or peripheral neuropathy, patients often feel numbness/tingling/pain in the hands, feet and/or torso. If amyloid affects the nerves that control organ function (also known as autonomic nerves), the patient may experience dizziness or loss of consciousness when standing up, diarrhea, constipation, or sexual dysfunction in males.
Soft tissue: Patients with amyloidosis may develop carpal tunnel syndrome (numbness and tingling of the hand in a certain distribution) if amyloid deposits in the soft tissue of the canal where a nerve supplying the hand is. As this condition worsens, the patient may develop weakness or pain in the hand.
Gastrointestinal system: Amyloid can deposit anywhere in the digestive system. This can lead to weight loss, bloating, nausea/vomiting, bleeding in the intestines, and difficulty swallowing. Other symptoms such as diarrhea or constipation can occur due to involvement of the nerves supplying the gut.
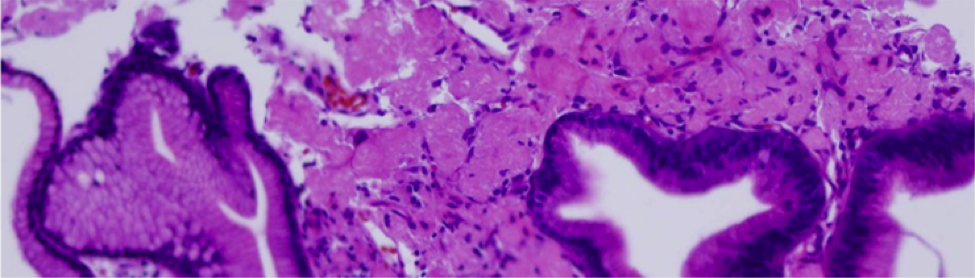
Figure 3: Stomach biopsy with amyloid deposits. Photo provided by Dr. Stephen Cook.
Coagulation System: In certain patients, the presence of amyloid may interfere with the normal coagulation process. The patient can develop easy bruising and spontaneous bleeding.
Other symptoms: Patient may also have enlargement of the tongue, voice hoarseness, bruising around the eyes and skin/nail changes.
The abnormally folded proteins in systemic light-chain amyloidosis are the light chains of antibodies. This is considered a type of blood cancer because the factory that is making the light chains is typically a plasma cell cancer (Figure 4) or sometimes a lymphoma. A bone marrow biopsy is important to assess what type of cancer is producing the light chains. Other tests used to evaluate the disease include serum protein electrophoresis, serum immunofixation, serum free light chains, urine protein electrophoresis and urine immunofixation. In addition, light chain amyloidosis patients often have protein deposition in the heart and kidneys. Other organs affected may include the gut, nerves, coagulation system and/or soft tissues. When amyloid deposits in these organs, patients develop symptoms from organ failure. As such, a thorough evaluation of the heart and kidneys is commonly done at diagnosis. The evaluation may consist of an electrocardiogram, cardiac ultrasound, blood tests and a 24-hour urine study.
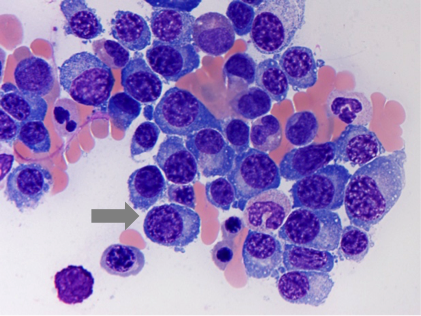
Figure 4: Bone marrow biopsy from MM patient. Arrow highlights malignant plasma cells. Photo provided by Dr. Karthik Ganapathi.
Treatment for this disease is aimed at eliminating the cells that are making the light chains, i.e. “shutting down the factory”. Once the factory has been shut off, this allows the body to heal. Because the factory is a cancer (see above), treatment consists of chemotherapy. Because the factory producing the light chains is often times a plasma cell cancer, treatment of this disease is similar to another type of plasma cell cancer, called multiple myeloma. The drugs used may include a combination of chemotherapy [cyclophosphamide, melphalan], proteasome inhibitors [bortezomib, carfilzomib], immunomodulatory drugs [lenalidomide, pomalidomide] and corticosteroids. Certain patients may also be eligible for an autologous stem cell transplant as another way to treat this cancer.